Seasonal Allergies, Sleep Apnea, and CPAP Problems
Nasal congestion, a runny nose, sneezing, watery eyes, a scratchy throat these are just a handful of the symptoms that come with springtime allergies. Suffering through these symptoms is an unpleasant inconvenience in ordinary circumstances. But if you use CPAP therapy, allergies are more than just unpleasant. Seasonal allergies can actually make your sleep apnea worse and treating it with CPAP more challenging.
Seasonal Allergies and Apnea
When spring is in the air, so is airborne pollen from trees, mold spores, weeds, grasses, and of course the spectacular, colorful flowers you see bursting up in gardens and at the sides of the road.
Unfortunately, for about 50 million Americans, the joyous end of winter ushers in a new season: allergy season. If you suffer from seasonal allergies, all that pollen in the air signals your body to release histamine to conquer the invading particles. This is why you start sneezing, coughing, and your eyes start watering: your body’s trying to expel and fight off the enemy.
Increased histamine levels also causes inflammation of the nasal passages. You probably know this as the classic stuffed-up nose and sinus headache combo. You may have facial tenderness around the cheeks and nose, a completely blocked nostril, or an annoying wheezing and whistling as air struggles to pass in and out of your nose.
Many people with swollen nasal passages mistakenly believe that if they blow their noses long enough, they’ll make room for air and get some relief. But if you tilt your head back and look up your nostrils in the mirror, you may notice that its the swelling of your nasal passages themselves not necessarily the presence of heavy mucus thats preventing you from breathing easily.
Hay fever and allergic rhinitis complicate sleep, of course. Not being able to breath through ones nose (or being kept awake by that annoying nose whistling) is a problem for those who aren’t comfortable mouth breathing.
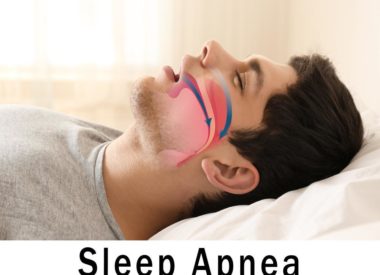
But it’s an even bigger concern for those with obstructive sleep apnea (OSA). All that swelling means your upper airway is narrower than normal. On top of that, mucus congestion shifts around when you lie down. When you’re standing or seated, gravity helps to drain your sinuses properly (ideally, into a tissue). When you switch to a prone position, the mucus is pulled deeper into your airway or down the back of your throat. This aggravates your existing apnea symptoms by making breathing even more difficult than normal. If you cant breathe through your nose, you cant get the full benefit of your CPAP therapy. You’ll probably try to compensate by breathing through your mouth, which can be a problem if your mask doesn’t cover your whole face.
For snorers who don’t use CPAP or apnea therapy of any kind, you’ll see a difference, too. Snorers with allergies will almost certainly snore more (and more loudly). In fact, many people who don’t normally snore find themselves picking up the habit temporarily until their airway swelling subsides.
If you have apnea, seasonal allergies can present a real problem. If allergies interfere with your sleep quality (as allergic rhinitis does for about half of all people who experience it), they’re likely interfering with your breathing and your apnea therapy, as well. And as people with apnea know, stopping CPAP therapy or CPAP therapy that fails for some reason can have many negative health effects, both in the short term and long term.
Daytime sleepiness, fatigue, poor cognitive skills, memory and concentration problems, headaches, high blood pressure, and problems regulating your appetite and hunger are just a few health concerns that go hand-in-hand with reduced CPAP therapy effectiveness.
Seasonal Allergies and CPAP Problems: Treat Your Symptoms First
The best way to maintain your CPAP effectiveness when you’re suffering from allergies is to address the underlying allergy itself. If you have seasonal hay-fever or allergic rhinitis, you can take some simple steps to help reduce your allergies and treat their symptoms.
- Limit your exposure to pollen. Though its frustrating to stay indoors on a beautiful day (and difficult to avoid all allergens all the time), you can improve your symptoms by going outside when the pollen count is a bit lower. Times to avoid being outdoors: early mornings (when the pollen count is at its peak), windy days, dry days.
- Keep your home allergen-free. Vacuum and dust regularly to keep the presence of indoor allergens to a minimum. Wash your bed linens frequently, too, and dry them (and your clothes) indoors instead of on a clothesline. Keep windows and doors shut. If you run air conditioning or forced air heat, make sure your filters are fresh and properly functioning.
- Keep pets out of bed. Keeping your dog or cat out of your bed is good sleep hygiene at all times of the year. But if Fido or Mr. Whiskers is an outdoor pet, its particularly important to banish him during allergy season. Pollen on hair or fur can get transferred to your sheets and pillows, making your symptoms worse.
- Change out of outdoor clothes. If you’ve been outside doing yard work or exercising, change into fresh, clean clothes when you come back indoors.
- Using a humidifier by your bed at night can help put moisture into the air. (Dry nasal passages can make congestion worse and can lead to nosebleeds.) Taking hot showers or using a steam bath may also help to clear your sinuses.
- Take oral antihistamines and decongestants. Check with your doctor first, especially if you’re taking other medications. Over-the-counter products like loratadine (generic Claritin) or phenylephrine (generic Sudafed) may work fine, but some people benefit from prescription allergy medicine. Be careful when taking non-drowsy drugs close to bedtime; these often contain stimulants that can keep you awake.
- Use a saline spray. These sprays, which you can buy over-the-counter at a drugstore, help to reduce nasal swelling. Prescription and prescription-strength sprays (like Fluticasone Propionate, or Flonase, which is a glucocorticoid) are also available.
- Try a nasal wash or neti pot. Rinsing your nasal passages with a mix of water and salt may help to flush allergens from your nose and reduce swelling.
- Wear Breathe-Rite strips when you sleep. These adhesive strips affix to your nose and help to widen nasal passages, allowing air to move more easily through the upper airway. In some cases, using a nasal strip in conjunction with CPAP therapy may be sufficient to address breathing difficulties from allergies.
Allergies and CPAP: Make Your Mask Work for You
Some people with apnea may be tempted to stop using CPAP until their allergies go away. This would be a mistake. For one, its never wise to stop your treatment, even for a day if you can avoid it. But also, continuing with your therapy provides a huge benefit that can actually help improve your allergy symptoms: the humidification chamber.
The job of the CPAP humidifier is to provide moisture to your nasal passages and upper airway. Moist nasal passages are less likely to trigger sneezes. If your nose and sinuses are kept lubricated, your body doesn’t need to provide as much mucous, either. Using the humidifier is a win-win: it makes your apnea therapy more effective (and comfortable) and it gives your body extra support when dealing with allergies during sleep. Typical allergy symptoms like a dry, scratchy throat, a cough, a runny nose, or an attack of sneezes will be less likely to wake you in the night.
However, even with the CPAP humidifier on, allergy sufferers with apnea may still have trouble breathing. If you’ve tried all the above techniques and you’re still having difficulty getting enough oxygen, switching from a nasal pillow or nasal-only style mask to a full face mask may help. Full-face masks provide adequate air pressure to keep your airways open whether you’re breathing in through your nose or mouth (or both). Once your allergy symptoms have resolved, you can switch back to your preferred mask style.
A second option is to talk to your sleep specialist about trying APAP (automatic positive airway pressure) therapy. Whereas CPAP machines provide a continuous, steady air pressure, APAP operates across a range. If your pressure needs increase while you’re asleep for example, when your breathing is completely blocked by inflamed nasal passages the APAP can detect this and raise its level of pressure to force air past the blockage.
The important thing to remember is that you have options. By communicating with your regular physician and your sleep physician, you can come up with a strategy for overcoming allergy symptoms and improving your quality of sleep. Remember: allergy season isn’t always predictable. It can last anywhere from a few weeks to a few months. Having a plan for continuing your therapy uninterrupted is a smart investment in your overall health.