Adaptive Servo Ventilation (ASV) and Central Sleep Apnea
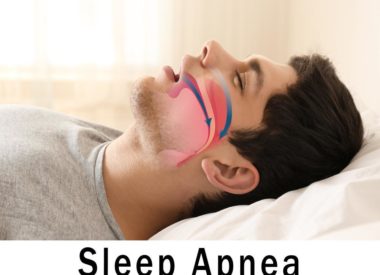
Recently we also introduced central sleep apnea syndrome (CSAS), a different kind of sleep apnea which occurs when the brain fails to signal to the respiratory system that it needs to continue breathing during sleep.
CSAS is not a problem of mechanics, like OSA. Instead, it is a neurological problem. It can lead to recognizable patterns of shallow breathing, or to partial or complete episodes of apnea.
Often, central sleep apnea happens as a result of other underlying health conditions (such as congestive heart failure) or due to adverse side effects from the use of certain medications.
To understand how treatment for CSAS can be different than for OSA, it’s important to differentiate between forms of noninvasive ventilation therapy.
A review of noninvasive ventilation therapies
For all forms of sleep apnea, treatment involves some form of noninvasive ventilation. These devices draw in air from the room, then pressurize it based on programmed settings inside the machines. The machines come in small boxes that enclose fans, motors, and humidifiers, with tubing connected to a mask to deliver the therapy. The therapies include PAP and ASV.
Positive Airway Pressure (PAP)
The machines that provide noninvasive ventilation include the different forms of positive airway pressure (PAP) therapy and adaptive servo-ventilation (ASV) therapy.
- CPAP stands for continuous positive airway pressure. It offers a single fixed pressure setting to counteract and prevent obstructive breathing patterns. Its the gold standard for treating classic OSA.
- Automatic PAP (or APAP) is preset to a specific minimum and maximum pressure range which is programmed to fluctuate in order to deliver the perfect pressure, breath by breath. It is also used mostly for treating OSA.
- BiPAP, or bi-level positive airway pressure, works for patients with more severe OSA who must address higher pressure needs. BiPAP creates an ideal duo of pressures: one for inhalation, another for exhalation. This provides extra comfort and offers the option of presetting the breathing pattern to a timed or spontaneous backup rate. This allows a temporary increase in air pressure to smooth over any breaks.
BiPAP with backup rate is also often used as the first line of therapy for central sleep apnea. If it doesn’t provide the relief and support these patients need, then ASV is introduced as a different option for noninvasive ventilation.
Adaptive Servo-Ventilation (ASV)
ASV does not appear, on the surface, to be any different than PAP. However, its the technology behind the pressure delivery that makes it unique.
ASV is considered a smart device. It is programmed with algorithms which anticipate and detect major changes in breathing patterns; it senses these shifts and intervenes with just enough positive airway pressure to help maintain the patients breathing at 90 percent or better of what that patients normal pattern resembled prior to episodes of abnormal respiration.
The algorithms are based off the breath-per-minute pattern of each individual patient and set to support an ideal rate. If, as the patient is using ASV, their breathing pattern dips below this rate, the ASV kicks in and makes a temporary pressure change to help the patient stay on a regular respiratory course.
The primary patients who qualify to use ASV:
- have CSAS that has been shown to be non-responsive to BiPAP with backup rate
- have mixed sleep apnea (in which both CSAS and OSA coexist)
- may have developed mixed sleep apnea after beginning PAP therapy for OSA
- have a specific kind of abnormal breathing pattern called Cheynes-Stokes Respiration (CSR)
CSR is an abnormal sleep breathing pattern with a central origin. It resembles a waxing and waning wave pattern (see left), which crescendos into stretches of deep (and sometimes fast) breathing followed by patterns in decrescendo that lead to very shallow respirations and, eventually, episodes of apnea.
Because CPAP and APAP cannot be preset to accommodate such complex sleep breathing patterns, they are not typically useful to patients with central sleep apnea, mixed sleep apnea, or CSR.
How to begin a trial of ASV
Despite the machines smart technology, the ASV still requires that the patient use it in a lab environment overnight. This is so that the patient’s baseline breathing patterns can be established (for both minimum and maximum pressure support settings). The proper setting for oxygen support is also determined for programming into the custom calibration afterward.
Who is disqualified from usingASV?
In 2015, the Serve-HF study found that ASV was no longer a safe choice for a very specific subset of patients who suffered from chronic heart failure. These patients experience a symptom known as left ventricular ejection fraction(LVEF); its severity is expressed as a percentage.
Patients with chronic heart failure who have a reduced LVEF of less than or equal to 45 percent were at 33 percent higher risk for cardiovascular death than patients with similar symptoms who were not using ASV.
Patients who are considered candidates for ASV by sleep physicians are typically screened by cardiologists for these important factors to determine if the technology is safe for them to use. If ASV is not recommended, alternatives are best determined by the sleep physician.