What is an Overnight Sleep Study (Polysomnogram)?
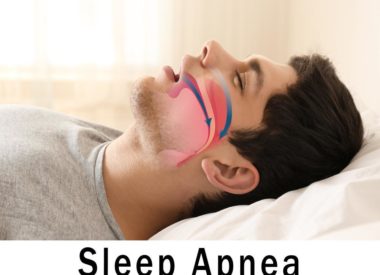
If your doctor suspects you have a sleep disorder like sleep apnea, sleep related movements, or narcolepsy, he or she may refer you to a sleep center for an overnight sleep study, or polysomnogram. The purpose of this sleep study is to monitor you while you sleep, to get a more complete picture of whats happening in your brain and to your body.
The goal of a sleep study is to determine whether you have a sleep disorder, and if so, to diagnose which one, so you can treat it and finally get a restful and restorative sleep.
What is an overnight sleep study test?
An overnight sleep study test, or polysomnogram, is also called a nocturnal polysomnogram (NPSG). Nocturnal means it happens at night. Polysomnogram means it measures many different body functions while you’re asleep, including:
- heart rate
- brain activity
- oxygen levels
- eye movements
- airflow
- respiratory effort
- body movement
The purpose of a nocturnal sleep study is to use the above data to diagnose and treat sleep and arousal disorders.
At your overnight sleep study, trained sleep technologists lead you through the process and monitor the equipment that records all of your sleep data into a digital diagnostic system. These technicians (sometimes called sleep techs) have specialized credentials: they are Registered Polysomnographic Technologists (RPSGT).
Sleep technologists, like your referring physician, are sleep medicine professionals who work directly with your doctor to make sure you’re properly and accurately diagnosed and treated. Their work with you begins with your sleep study and sometimes continues after, with ongoing patient education and treatment. (For example, if you are diagnosed with sleep apnea, you may make continued visits to the sleep lab for CPAP fittings and follow-up visits.)
At your sleep study, you don’t need to do a thing except sleep; the lab technicians record the data. By monitoring the real-time data coming in from your wires and sensors and from in-room video, they can see how your body behaves through all the stages of sleep.
A sleep study can reveal any abnormalities in your sleep patterns; for example, if you snore, experience apneas (cessation of breathing), have any involuntary movements (like leg motions or sleepwalking), or spend too little time in any of the stages of sleep.
Whats involved with a sleep study
If all of this is new to you, you’re probably wondering what to expect from a sleep study. Though sleep labs vary, your experience should be something like this:
- First, your physician will recommend that you visit a sleep clinic for a sleep study. Once the study is approved by your insurance as medically necessary, you’ll get a referral to a sleep center (sometimes called a sleep clinic or sleep lab).
- When you call to make your sleep study appointment, the clinic will ask you questions about your sleep and any medications you’re taking. They’ll also advise you as to how to prepare for your sleep study. For example, you may be instructed to refrain from taking certain medications. You’ll also be advised to not drink caffeine or take a nap on the day of your polysomnogram. Technicians will also ask that your hair be dry and that you not put any styling products in it, as these can affect the sensors.
- When you arrive for your sleep study, pack as if you’re going to a hotel. Bring an overnight bag with comfortable pajamas and something to wear in the morning. Bring whatever you need for your usual sleep ritual, such as as a book light and a book to read before bed. You can bring a pillow from home. You should also bring any medications you need to take. (Be sure to tell your sleep technicians about this medication in advance and again when you check in.)
- Overnight studies usually begin in the evening (between 5:30 PM and 9:30 PM) and end early in the morning (around 5:30 or 6:30 AM).
- After you check in for your study, you’ll be given a chance to change into pajamas. Then you’ll be brought to a private room to sleep. These rooms usually have a bed, a bedside table with a lamp, and oftentimes a TV.
- Your sleep technician will help use an adhesive to temporarily attach sensors and wires to your head and body at least twelve electrodes (flat metal discs), and probably more. All wires are long enough to allow you to move around in bed as you normally would. You’ll also wear an elastic belt around your chest to measure breathing and a fingertip or earlobe clip to monitor heart rate and oxygen levels.
- Your sleep technician will also advise you as to how to use the bathroom in the night. A technician can help you to attach a portable device so your test is not interrupted by natures call. Alternately, your technician may show you how to unplug from, and reattach to, a central box so you can get up when you need to.
- All of these devices record your bodily functions and input the data into a digital diagnostic system, where your sleep techs can monitor readings as you sleep.
- Once your tech has set you up, he or she will ask you to test the connections by making some movements (for example, closing your eyes or moving your arms and legs).
- After that, you’ll relax in bed as you normally would, by reading or watching TV until you feel sleepy. When you’re ready, you can shut off the lights and go to sleep as you normally would at home.
- From the moment you’re hooked up to your equipment until the moment your awakened in the
morning, sleep technicians will monitor your vital signs and the various channels of data being transmitted to them. Techs collect and analyze this data, taking note of any irregularities as you pass through the stages of sleep (stages 1, 2, 3, and REM sleep).- A typical sleep study will have you hooked up to an electrocardiogram (EKG), an electro-encephalogram (EEG), an Electrooculography (EOG), and an Electromyography (EMG). Thesemonitor heart and brain activity, eye movement, and muscle activity.
- Other sensors will monitor your snore volume, your breathing, your body position (for example, if you sleep on your back or side), and your blood oxygen saturation. These sensors help to determine if your breathing is interrupted and if you’re getting enough oxygen to your brain. They also help to associate any changes in your sleep with your body’s position at the time.
- Sleep techs will also watch video of you as you sleep. This video is recorded to help check your body position against the recorded data. Its also useful for documenting any seizures or movements you make while asleep.
- During the night, its possible the sleep tech may awaken you and ask you to sleep on your back or to otherwise change position. This request is usually for the purpose of gathering clearer data.
- If your sleep technologist sees you having instances of sleep apnea, he or she may come into your room and fit you with a CPAP facial mask. In this case, you will be asked to try and sleep with the CPAP therapy so the technologist can get a reading of how you respond to it.
- In the morning, a technician will come wake you up. At this time, you simply get dressed and go about your day.
Many people worry that they wont be able to fall asleep or stay asleep at an overnight sleep study. However, the rooms are designed to be restful and relaxing. Though your sleep may not be as good as usual, most patients sleep for at least part of the night, which is enough for the technologists to gather the information they need.
Getting Your Sleep Study Results
Your technologists will need to compile and review the collected information from your test. They then provide it to the sleep centers board-certified sleep specialist, who reviews it and makes a diagnosis based on the results of the study combined with your medical history.
If a different doctor (for example, your primary care physician) ordered the sleep study, he or she will be sent a copy of the results for review with you.
After an average of about two weeks, you’ll be called to schedule a follow-up with your sleep medicine doctor. At this time, he or she will go over your results and diagnosis and determine a treatment plan.