Check out these solutions for 6 common problems with CPAP (Part One)
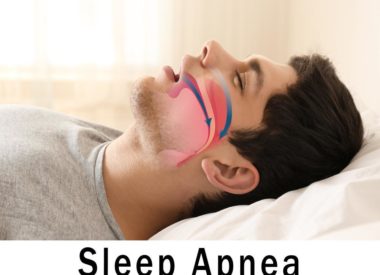
Continuous positive airway pressure (CPAP) therapy is considered the gold standard for treating sleep apnea (especially obstructive sleep apnea, or OSA).
However, while some people take to this therapy just fine, it may be more problematic for others.
Here’s a guide to 6 key complaints from CPAP users and some basic solutions, divided into a 2-part series.
Solutions to 6 common problems with CPAP (1 – 3)
While this list doesn’t exhaust all the potential obstacles you may face while treating sleep apnea, it does capture the 6 most common problems that CPAP users encounter. Here are 3.
#1: You can’t fall asleep while wearing the mask
This could be caused by any of the following:
-
The machine (or mask) makes noise. Current models of CPAP machines barely make a sound, so if yours is loud, it may not be working properly. If your mask is making friction noises, it is probably not “seated” on your face correctly, or it may be the wrong style or size. Let your DME know about noise issues with either so they can offer you suggestions for correcting the problem.
If it’s just a case of noticing some noise (some people equate the sound of CPAP to background or “white” noise), it might be simply a case of adjusting to the new sound in your environment.
-
You can’t get used to feeling it on your face. It’s normal for first-time users to be self-conscious of the way CPAP masks feel on the face. However, it’s not normal for themto feel uncomfortable or painful.
If you practice wearing it without using the therapy during the day (such as while watching TV or knitting or listening to music), you will eventually get used to the feeling of it against your skin. This is called desensitizing .
However, if it just feels painful or irritating, no matter how hard you try to adjust, it may simply be the wrong mask. If this is the case, call your DME and tell them your situation. You aren’t stuck with the first mask you try; there are many to choose from and there’s definitely a mask for every situation out there.
-
It gives you feelings of anxiety or claustrophobia. Some people cannot keep the mask on for more than a couple of seconds before they quickly pull it away from their face. They try to desensitize as described above, but within seconds, they give up.
Claustrophobia and anxiety are linked to issues unrelated to sleep apnea. You may benefit from seeing a professional who specializes in cognitive behavioral therapy (CBT) to help you overcome your anxiety or claustrophobia.
You might also try practicing relaxation exercises before bedtime to reduce those feelings. A switch from your current mask to one that uses less headgear or makes you feel more comfortable could be a good solution. Some people may also use a mild anti-anxiety medication in order to move past their anxiety.
In any event, you need to contact your DME about your concerns; an unworn CPAP mask makes your therapy useless, and you still need to find a way to treat your sleep apnea.
-
Your pressure seems too high. For those with moderate to severe sleep apnea, launching into therapy set at a higher pressure may make it difficult to fall asleep.
You can try to practice controlled breathing at first, to see if focusing on your inhalations and exhalations in a steady, calm pattern can help you adjust (try this for about 10 minutes).
You likely have a machine that offers something called a ramp feature. This feature starts your therapy at a lower pressure while you are still awake, then slowly increases your pressure so that, by the time you do fall asleep, it’s where it needs to be. If you don’t know how to use your ramp feature, your DME would be happy to show you how it works.
#2: You experience dry mouth, dry eyes, or dry nose
These are common occurrences, but they can be corrected by understanding what causes them.
Dry mouth
This is typically caused by oral breathing (more commonly referred to as mouth breathing). The pressurized air shoots into the nose, then is funneled right back out through the open mouth, leaving the tongue, gums, and other tissues vulnerable to dryness.
People with sleep apnea often develop the tendency to mouth breathe because that’s the way their body and brain have compensated for poor oxygen from breathing restrictions caused by apneas while sleeping.
If you are early into your therapy (less than a month), a dry mouth may be a sign your body is still relearning to breathe correctly at night. You can confirm you are doing this by looking at your leak readings; if you have unacceptable leak issues, it might be because of this (or it could be your mask fit).
If it becomes an ongoing problem, you can consider selecting a mask that covers both the mouth and nose to make the problem moot. Or you can ask for a chin support, which attaches to the headgear and gently coaxes the mouth shut. This may be all that’s need to retrain yourself to breathe through your nose, and may be something you only use temporarily.
Dry eyes
Air leakage at the top of the mask can lead to dry, irritated eyes. The air blows into the interior corners of your eyes and dries them out. If not addressed, this can lead to bigger problems with the eyes later, so don’t ignore it.
The best remedy is to adjust the mask to fit better across the bridge of the nose.
However, this doesn’t mean over tightening the mask; to the contrary, an overtightened mask will torque, breaking the seal and leaking air.
If you can’t get your mask to fit your face properly, talk to your DME. You might need to find a different shape or size to fix the leak issue.
Dry nose
Many people experience raw, dried-out nasal tissues after using CPAP therapy. Most machines now come equipped with humidifiers, so it may be that you aren’t using your humidifier, it’s not working correctly, it’s turned off, it’s set too low for comfort, or it may not be heated (which helps provide additional comfort).Ask your DME for help if you think the problem is related to humidification for CPAP.
You can also try a saline nasal spray just before bedtime to moisten the nasal passages; there are also nasal steroid sprays available by prescription if dry nose is a constant problem.
Finally, make sure your mask fits properly. Leaky masks (no matter where the air leaks) can lead to dried nasal tissue as well.
#3:You’re congested
Stuffy noses usually result from problems with the CPAP humidifier. Either it’s turned off, turned down too low, or isn’t filled with enough water to generate enough steam for the whole night. It could also simply be defective.
It helps to use the heated feature as well; warmer air is more soothing to the nasal passages than cooler air. Ask your DME to help you with your CPAP humidification if you wake up stuffy, sneezing, or with a runny nose.
Some people also have structural problems with their nasal and sinus passages. They may have nasal polyps, a deviated septum, swollen turbinates, or other issues that can be addressed by an ear, nose, and throat specialist.
People with allergies may also experience some of these concerns.
In any case, make sure you communicate these problems to your DME or your doctor to make sure CPAP is right for you.
If you have experienced any of these problems, and have tried these solutions without success, we highly recommend you contact your durable medical equipment (DME) provider (they are the ones who arranged for the delivery and set up of your CPAP therapy equipment).
Even those who are most challenged to make CPAP work can benefit from a discussion with the DME, who has specific training in the art of troubleshooting problems with therapy. They have seen nearly every kind of troublesome situation and can be invaluable in addressing your problems, usually with simple and inexpensive tactics.
Are you a Sound Sleep Health patient? Let us help you with your CPAP therapy success! Call our DME for advice at 425.279.7151 if you face these or other obstacles with the use of your CPAP therapy.