What is the best sleep study for my problem?
There are dozens of sleep disorders that require some form of testing in order to identify and treat them. Here are the most common sleep studies being performed in sleep centers. The best sleep study for you is likely going to be one (or more) of these.
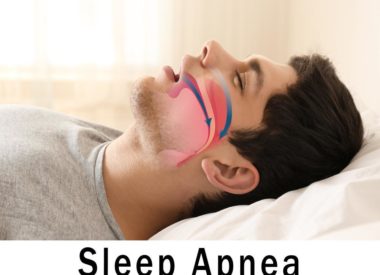
The home sleep apnea test (HSAT)
Also referred to as the home sleep test (HST),this test involves a minimum of recording sensors that the patient administers in the privacy of their own home. It usually includes belts that measure breathing effort, airflow sensors applied to the nose and/or mouth, and a finger clip that records both heart rate and the amount of oxygen in the bloodstream at any given time.
The HSAT is fairly inexpensive and used primarily as a means for ruling in or ruling out certain kinds of sleep disorders. The patient is typically shown how to set up the test while at the sleep center, or is given illustrated written instructions or a video to take home for guidance.
At bedtime, the patient applies the sensors, turns on the test and goes to bed. In the morning, they turn off the test and remove the sensors. Multiple nights of sleep testing at home are sometimes required to get the most accuracy portrait of the patients sleep architecture and respiratory patterns. The patient then returns the test kit to the sleep center so that the data it has recorded can be downloaded, reviewed, and interpreted.
The test records key data that is reviewed at the sleep center after the equipment is returned. From the test data, the doctor then determines the likelihood that the patient has a sleep-breathing problem or other sleep health concern. They will make recommendations at that time.
The HSAT is not indicated for all patients, so this may or may not be the right test for you. Patients with other serious medical concerns do not qualify for this test and must participate in what is known as an attended overnight sleep test at the sleep center.
Overnight attended sleep studies
There are three kinds of overnight sleep tests that take place in the sleep center. They are attended, which means a sleep technologist will prepare patients for these tests, attend the data overnight as it livestreams during the test, and assist the patients throughout all aspects of the study.
These kinds of tests record comprehensive amounts of biological data that can help the sleep specialist identify with more precision, accuracy, and certainty the reasons for their patients sleeping struggles. These tests are more accurate than HSATs because they measure more key biological processes and, if a sensor should fall off, the sleep technologist can easily reapply it, preserving the accuracy of the study. This explains why attended studies more expensive.
Overnight attended studies also introduce the patient to the common technology known as CPAP (or continuous positive airway pressure) by showing the patient how the mask fits, what the machine does, and how positive air pressure can work to correct sleep-breathing disorders.
The basic overnight study: NPSG
NPSG stands for nocturnalpolysomnogram, and it is the most basic form of the overnight test. The patient arrives, is hooked up to myriad sensors by the sleep technologist, then put to bed in a comfortable sleeping space.
The sleep technologist records several different kinds of data, including leg movements, breathing patterns, eye movements, brainwave patterns, heart rate and cardiac waveforms, blood oxygen levels, airflow through the mouth and nose, chin activity, even body positioning and snoring.
Once the test is over, the technologist awakens and unhooks the patient, allows them to shower, and gives them instructions for what happens next. Meanwhile, the data they have collected (which on paper usually equals about 800 pages) is scored and a report of its details is generated.
The physician reviews this report, interprets the results, then consults with the patient to go over the findings in a separate meeting after the test has taken place.
The Split Night Study
The split night study is similar to the NPSG in that it starts out in the same way. However, the doctor may have high suspicion that the patient has moderate to severe obstructive sleep apnea (OSA). They may have seen evidence of it on a prior HSAT, for instance, or the patient may have several risk factors that make them more predisposed to sleep breathing problems.
If this is the case, the physician pre-assigns an order to the technologist. After a specific time has passed in the study, if the patient is showing evidence of a sleep-breathing disorder which meets prearranged criteria for treatment, the technologist is permitted to initiate a trial of therapy using CPAP. All of the sensors stay put except for the airflow measurements, which the CPAP machine takes over when it’s applied.
A study that measures the patients responses to CPAP is called attrition. For moderate to severe apnea patients in a split night study, the urgency of their condition may warrant starting them right away on a CPAP titration in order to efficiently identify what that patients unique positive airway pressure setting will be without requiring that they come back for a second night.
During the titration, the sleep technologist adjusts air pressure, humidity, and comfort settings throughout the test in order to effectively treat obstructions as they arise, ideally until they are resolved.
The split night study also provides a good opportunity for the patient to trial one or several mask types or brands to find the perfect fit. At the end of the night, the patient is unhooked and the test data is collected, scored, reviewed, and interpreted by the physician.
The outcome of this test will be discussed between the patient and the physician, who will make recommendations based on the data.
Positive Airway Pressure (PAP) Titration
A PAP titration requires the same set up as the NPSG, but the patient starts out using CPAP from the very start. This test also provides opportunities for patients to trial different masks. Like the titration in a Split Night Study, the sleep technologists spends the night adjusting the pressure and recording data to ensure that apneas have been resolved. At the end of the study, a final recommendation about the patient’s best pressure setting is determined in the report that goes to the physician. The patient is unhooked and the test is collected and sent on for scoring and interpretation by the physician.
The outcome of this test is that the patient will receive a therapy strategy that includes equipment set up and directions for how to begin using the newly prescribed air pressure at home.
In some cases, patients who qualify for alternatives to CPAP, such as oral or dental devices, may be instructed to meet with a board-certified dentist, who will handle the manufacture and fit of an appliance that can help improve their sleep-breathing problems. These often require follow-up studies to measure their effectiveness, sometimes at home and sometimes at the lab.
Nap testing
There are two primary daytime tests used in sleep centers, the MSLT and the MWT. They are called nap tests because they use naps (or resistance to naps) as measures of daytime sleepiness.
Multiple Sleep Latency Test (MSLT)
The MSLT is a daytime test which is used to measure how easily patients can fall asleep during the day. It is performed on patients who experience profound levels of daytime sleepiness and symptoms that suggest narcolepsy or hypersomnia. It is also performed during the day to measure the effectiveness of a patients therapy for a preexisting sleep-related breathing disorder.
The patient will undergo 4 to 5 short (20-minute) nap tests throughout the day, usually following an overnight sleep test which has conclusively ruled out sleep apnea or movement disorders of sleep as the underlying cause of their chronic drowsiness.
Some of the sensors used on the patient during the overnight tests will be removed as they no longer are necessary, such as the respiratory belts and the airflow equipment. After the last tests are performed, the patient is unhooked and sent home.
Meanwhile, the data from this test is scored, reported, and reviewed by the physician, who will meet the patient at a later date to discuss results.
It is important to note that for those undergoing this test, the physician may ask that certain kinds of maintenance medications be suspended for a specific period of days prior to MSLT in order to rule out drug side effects and other reasons that could account for extreme daytime sleepiness in the patient.
The Maintenance of Wakefulness Test
The MWT is another daytime test which measures the opposite of the MSLT: how difficult it is for the patient for stay awake during the day while in a relaxing, stimulation-free environment. It is commonly used to confirm the effectiveness of the patients CPAP, dental or oral device, or medication therapy, or for patients who may be suspected of driving or operating machinery while drowsy during the day.
In fact, the MWT is a common test required of workers in specific fields where long-periods of passive activity (such as assembly line work or any kind of vehicular driving) can result in safety issues is the workers are drowsy. Some employers now require that employees using therapies for sleep disorders have their therapy compliance checked and confirmed regularly to ensure their safety on the job.
Patients for MWT are hooked up to a limited set of sensors to measure heart activity, brain activity, and eye and chin movements. They are given this 40-minute test 4 to 5 separate times during the day in a dimly lit, quiet room where they are asked to remain calm and awake without the benefit of any stimulation to encourage wakefulness. Meals at typical mealtime hours are included in the test.
In between tests, which are spaced about 2 hours apart, the patient remains in the room and can move about freely, watch TV, read a book, or otherwise keep themselves company. The tests are ended earlier if, during any single test, the patient falls asleep during any of the 40-minute trials.
After the MWT concludes, the patient is unhooked and, again, their data is sent on to be scored and reviewed, with the physician consulting the patient at a later date on the findings.
What is the best sleep study for you?
It depends upon your history, symptoms, and situation. The only way to know which will best serve your needs is to consult with an accredited sleep physician, who must write the order for the test in order for it to take place. Every patient is unique, so the test (or tests) that one patient might undergo may vary dramatically from the test (or tests) of another patient.
Please reach out to us at Sound Sleep Health. We have 3 locations in the greater Seattle/Kirkland areas. If you have concerns about your sleep health or that of a loved one, call us and Improve Your Sleep Today!